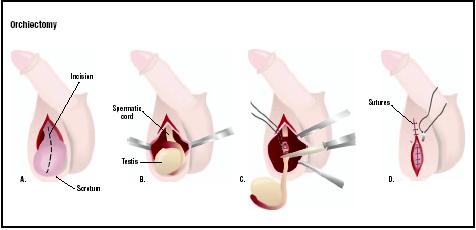
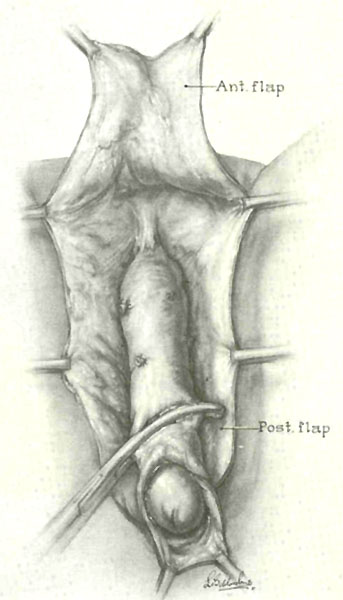
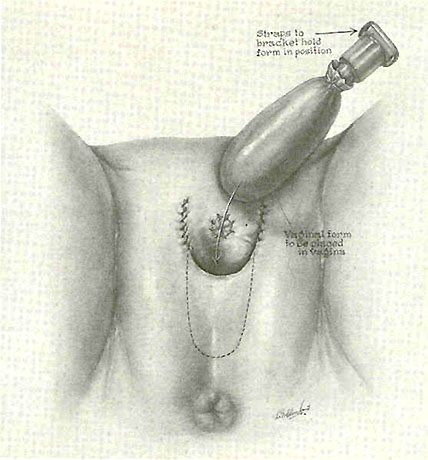
Orchiectomy is the surgical removal of one or both testicles, or testes, in the human male. It is also called an orchidectomy, particularly in British publications. The
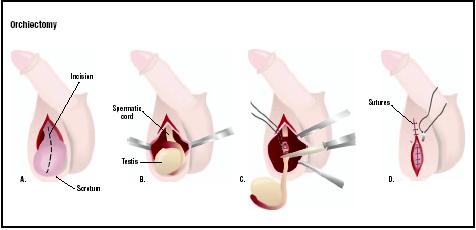
In an orchiectomy, the scrotum is cut open (A). Testicle covering is cut to expose the testis and spermatic cord (B). The cord is tied and cut, removing the testis (C), and the wound is repaired (D). (
Illustration by GGS Inc.
)
removal of both testicles is known as a bilateral orchiectomy, or castration, because the person is no longer able to reproduce. Emasculation is another word that is sometimes used for castration of a male. Castration in women is the surgical removal of both ovaries (bilateral
oophorectomy ).
Purpose
An orchiectomy is done to treat cancer or, for other reasons, to lower the level of testosterone, the primary male sex hormone, in the body. Surgical removal of a testicle is the usual treatment if a tumor is found within the gland itself, but an orchiectomy may also be performed to treat prostate cancer or cancer of the male breast, as testosterone causes these cancers to grow and metastasize (spread to other parts of the body). An orchiectomy is sometimes done to prevent cancer when an undescended testicle is found in a patient who is beyond the age of puberty.
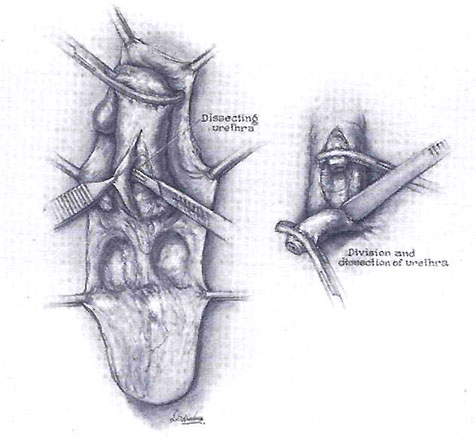
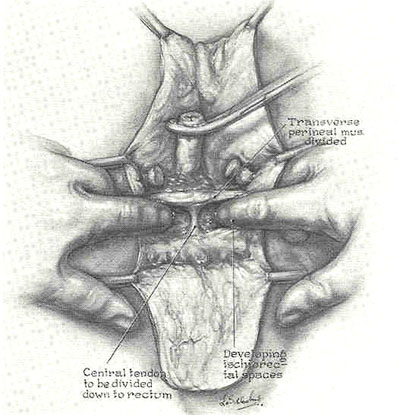
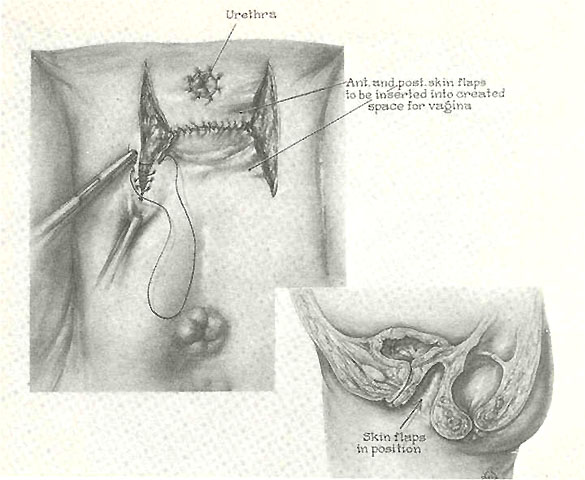
A bilateral orchiectomy is commonly performed as one stage in male-to-female (MTF) gender reassignment surgery. It is done both to lower the levels of male hormones in the patient's body and to prepare the genital area for later operations to construct a vagina and external female genitalia.
Some European countries and four states in the United States (California, Florida, Montana, and Texas) allow convicted sex offenders to request surgical castration to help control their sexual urges. This option is considered controversial in some parts of the legal system. A small number of men with very strong sex drives request an orchiectomy for religious reasons; it should be noted, however, that official Roman Catholic teaching is opposed to the performance of castration for spiritual purity.Demographics
Cancer
Cancers in men vary widely in terms of both the numbers of men affected and the age groups most likely to be involved. Prostate cancer is the single most common malignancy affecting American men over the age of 50; about 220,000 cases are reported each year. According to the Centers for Disease Control and Prevention (CDC), 31,000 men in the United States die every year from prostate cancer. African-American men are almost 70% more likely to develop prostate cancer than either Caucasian or Asian-American men; the reasons for this difference are not yet known. Other factors that increase a man's risk of developing prostate cancer include a diet high in red meat, fat, and dairy products, and a family history of the disease. Men whose father or brother(s) had prostate cancer are twice as likely as other men to develop the disease themselves. Today, however, there are still no genetic tests available for prostate cancer.
Testicular cancer, on the other hand, frequently occurs in younger men; in fact, it is the most common cancer diagnosed in males between the ages of 15 and 34. The rate of new cases in the United States each year is about 3.7 per 100,000 people. The incidence of testicular cancer has been rising in the developed countries at a rate of about 2% per year since 1970. It is not yet known whether this increase is a simple reflection of improved diagnostic techniques or whether there are other causes. There is some variation among racial and ethnic groups, with men of Scandinavian background having higher than average rates of testicular cancer, and African-American men having a lower than average incidence. Testicular cancer occurs most often in males in one of three age groups: boys 10 years old or younger; adult males between the ages of 20 and 40; and men over 60.
Other risk factors for testicular cancer include:
- Cryptorchidism, which is a condition in which a boy's testicles do not move down from the abdomen into the scrotum at the usual point in fetal development. It is also called undescended testicle(s). Ordinarily, the testicles descend before the baby is born; however, if the baby is born prematurely, the scrotal sac may be empty at the time of delivery. About 3–4% of full-term male infants are born with undescended testicles. Men with a history of childhood cryptorchidism are three to 14 times more likely to develop testicular cancer.
- Family history of testicular cancer.
- A mother who took diethylstilbestrol (DES) during pregnancy. DES is a synthetic hormone that was prescribed for many women between 1938 and 1971 to prevent miscarriage. It has since been found to increase the risk of certain types of cancer in the offspring of these women.
- Occupational and environmental factors. Separate groups of researchers in Germany and New Zealand reported in 2003 that firefighters have an elevated risk of testicular cancer compared to control subjects. The specific environmental trigger is not yet known.
Gender reassignment
Statistics for orchiectomies in connection with gender reassignment surgery are difficult to establish because most patients who have had this type of surgery prefer to keep it confidential. Persons undergoing the hormonal treatments and periods of real-life experience as members of the other sex that are required prior to genital surgery frequently report social rejection, job discrimination, and other negative consequences of their decision. Because of widespread social disapproval of surgical gender reassignment, researchers do not know the true prevalence of gender identity disorders in the general population. Early estimates were 1:37,000 males and 1:107,000 females. A recent study in the Netherlands, however, maintains that a more accurate estimation is 1:11,900 males and 1:30,400 females. In any case, the number of surgical procedures is lower than the number of patients diagnosed with gender identity disorders.Description
There are three basic types of orchiectomy: simple, subcapsular, and inguinal (or radical). The first two types are usually done under local or epidural anesthesia, and take about 30 minutes to perform. An inguinal orchiectomy is sometimes done under general anesthesia, and takes between 30 minutes and an hour to complete.
Simple orchiectomy
A simple orchiectomy is performed as part of gender reassignment surgery or as palliative treatment for advanced cancer of the prostate. The patient lies flat on an operating table with the penis taped against the abdomen. After the anesthetic has been given, the surgeon makes an incision in the midpoint of the scrotum and cuts through the underlying tissue. The surgeon removes the testicles and parts of the spermatic cord through the incision. The incision is closed with two layers of sutures and covered with a surgical dressing. If the patient desires, a prosthetic testicle can be inserted before the incision is closed to give the appearance of a normal scrotum from the outside.Subcapsular orchiectomy
A subcapsular orchiectomy is also performed for treatment of prostate cancer. The operation is similar to a simple orchiectomy, with the exception that the glandular tissue is removed from the lining of each testicle rather than the entire gland being removed. This type of orchiectomy is done primarily to keep the appearance of a normal scrotum.
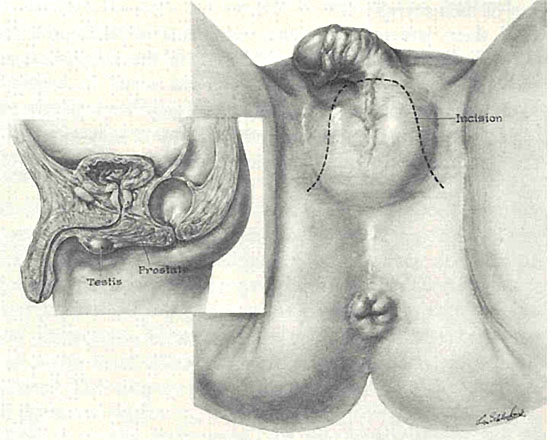
Inguinal orchiectomy
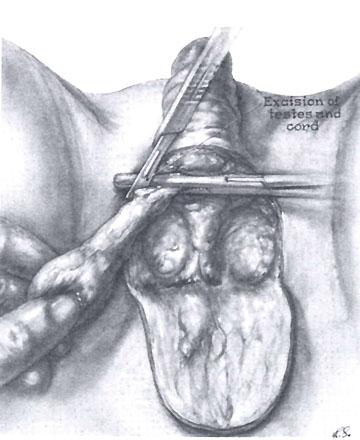
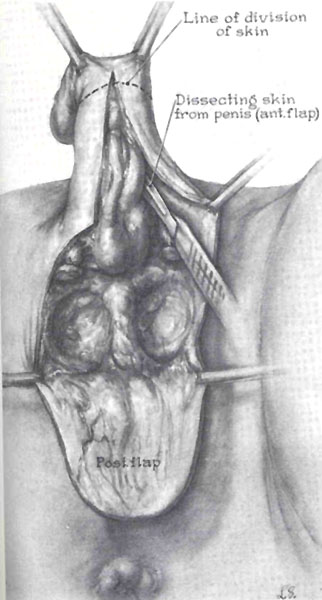
An inguinal orchiectomy, which is sometimes called a radical orchiectomy, is done when testicular cancer is suspected. It may be either unilateral, involving only one testicle, or bilateral. This procedure is called an inguinal orchiectomy because the surgeon makes the incision, which is about 3 in (7.6 cm) long, in the patient's groin area rather than directly into the scrotum. It is called a radical orchiectomy because the surgeon removes the entire spermatic cord as well as the testicle itself. The reason for this complete removal is that testicular cancers frequently spread from the spermatic cord into the lymph nodes near the kidneys. A long non-absorbable suture is left in the stump of the spermatic cord in case later surgery is necessary.
After the cord and testicle have been removed, the surgeon washes the area with saline solution and closes the various layers of tissues and skin with various types of sutures. The wound is then covered with sterile gauze and bandaged.
Diagnosis/Preparation
Diagnosis
CANCER. The doctor may suspect that a patient has prostate cancer from feeling a mass in the prostate in the course of a rectal examination, from the results of a transrectal ultrasound (TRUS), or from elevated levels of prostate-specific antigen (PSA) in the patient's blood. PSA is a tumor marker, or chemical, in the blood that can be used to detect cancer and monitor the results of therapy. A definite diagnosis of prostate cancer, however, requires a tissue biopsy. The tissue sample can usually be obtained with the needle technique. Testicular cancer is suspected when the doctor feels a mass in the patient's scrotum, which may or may not be painful. In order to perform a biopsy for definitive diagnosis, however, the doctor must remove the affected testicle by radical orchiectomy.
GENDER REASSIGNMENT. Patients requesting gender reassignment surgery must undergo a lengthy process of physical and psychological evaluation before receiving approval for surgery. The Harry Benjamin International Gender Dysphoria Association (HBIGDA), which is presently the largest worldwide professional association dealing with the treatment of gender identity disorders, has published standards of care that are followed by most surgeons who perform genital surgery for gender reassignment. HBIGDA stipulates that a patient must meet the diagnostic criteria for gender identity disorders as defined by either the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) or the International Classification of Diseases–10 (ICD-10).
Preparation
All patients preparing for an orchiectomy will have standard blood and urine tests before the procedure. They are asked to discontinue aspirin-based medications for a week before surgery and all non-steroidal anti-inflammatory drugs (NSAIDs) two days before the procedure. Patients should not eat or drink anything for the eight hours before the scheduled time of surgery.
Most surgeons ask patients to shower or bathe on the morning of surgery using a special antibacterial soap. They should take extra time to lather, scrub, and rinse their genitals and groin area.
Patients who are anxious or nervous before the procedure are usually given a sedative to help them relax.
CANCER. Patients who are having an orchiectomy as treatment for testicular cancer should consider banking sperm if they plan to have children following surgery. Although it is possible to father a child if only one testicle is removed, some surgeons recommend banking sperm as a precaution in case the other testicle should develop a tumor at a later date.
GENDER REASSIGNMENT. Most males who have requested an orchiectomy as part of male-to-female gender reassignment have been taking hormones for a period of several months to several years prior to surgery, and have had some real-life experience dressing and functioning as women. The surgery is not performed as an immediate response to the patient's request.
Because the standards of care for gender reassignment require a psychiatric diagnosis as well as a
physical examination , the surgeon who is performing the orchiectomy should receive two letters of evaluation and recommendation by mental health professionals, preferably one from a psychiatrist and one from a clinical psychologist.
Aftercare
Patients who are having an orchiectomy in an ambulatory surgery center or other outpatient facility must have a friend or family member to drive them home after the procedure. Most patients can go to work the following day, although some may need an additional day of rest at home. Even though it is normal for patients to feel nauseated after the anesthetic wears off, they should start eating regularly when they get home. Some pain and swelling is also normal; the doctor will usually prescribe a pain-killing medication to be taken for a few days.
Other recommendations for aftercare include:
- Drinking extra fluids for the next several days, except for caffeinated and alcoholic beverages.
- Avoiding sexual activity, heavy lifting, and vigorous exercise until the follow-up appointment with the doctor.
- Taking a shower rather than a tub bath for a week following surgery to minimize the risk of absorbable stitches dissolving prematurely.
- Applying an ice pack to the groin area for the first 24–48 hours.
- Wearing a jock strap or snug briefs to support the scrotum for two weeks after surgery.
Some patients may require psychological counseling following an orchiectomy as part of their long-term aftercare. Many men have very strong feelings about any procedure involving their genitals, and may feel depressed or anxious about their bodies or their relationships after genital surgery. In addition to individual psychotherapy, support groups are often helpful. There are active networks of prostate cancer support groups in Canada and the United States as well as support groups for men's issues in general.
Long-term aftercare for patients with testicular cancer includes frequent checkups in addition to radiation treatment or chemotherapy. Patients with prostate cancer may be given various hormonal therapies or radiation treatment.
Risks
Some of the risks for an orchiectomy done under general anesthesia are the same as for other procedures. They include deep venous thrombosis, heart or breathing problems, bleeding, infection, or reaction to the anesthesia. If the patient is having epidural anesthesia, the risks include bleeding into the spinal canal, nerve damage, or a spinal headache.
Specific risks associated with an orchiectomy include:
- loss of sexual desire (This side effect can be treated with hormone injections or gel preparations.)
- impotence
- hot flashes similar to those in menopausal women, controllable by medication
- weight gain of 10–15 lb (4.5–6.8 kg)
- mood swings or depression
- enlargement and tenderness in the breasts
- fatigue
- loss of sensation in the groin or the genitals
- osteoporosis (Men who are taking hormone treatments for prostate cancer are at greater risk of osteoporosis.)
An additional risk specific to cancer patients is recurrence of the cancer.
Normal results
Cancer
Normal results depend on the location and stage of the patient's cancer at the time of surgery. Most prostate cancer patients, however, report rapid relief from cancer symptoms after an orchiectomy. Patients with testicular cancer have a 95% survival rate five years after surgery if the cancer had not spread beyond the testicle. Metastatic testicular cancer, however, has a poorer prognosis.
Gender reassignment
Normal results following orchiectomy as part of a sex change from male to female are a drop in testosterone levels with corresponding decrease in sex drive and gradual reduction of such masculine characteristics as beard growth. The patient may choose to have further operations at a later date.
Morbidity and mortality rates
Orchiectomy by itself has a very low rate of morbidity and mortality. Patients who are having an orchiectomy as part of cancer therapy have a higher risk of dying from the cancer than from testicular surgery.
The morbidity and mortality rates for persons having an orchiectomy as part of gender reassignment surgery are about the same as those for any procedure involving general or epidural anesthesia.
Alternatives
Cancer
There is no effective alternative to radical orchiectomy in the treatment of testicular cancer; radiation and chemotherapy are considered follow-up treatments rather than alternatives.
There are, however, several alternatives to orchiectomy in the treatment of prostate cancer:
- watchful waiting
- hormonal therapy (The drugs that are usually given for prostate cancer are either medications that oppose the action of male sex hormones [anti-androgens, usually flutamide or nilutamide] or medications that prevent the production of testosterone [goserelin or leuprolide acetate].)
- radiation treatment
- chemotherapy
Gender reassignment
The primary alternative to an orchiectomy for gender reassignment is hormonal therapy. Most patients seeking MTF gender reassignment begin taking female hormones (estrogens) for three to five months minimum before requesting genital surgery. Some persons postpone surgery for a longer period of time, often for financial reasons; others choose to continue on estrogen therapy indefinitely without surgery.